Introduction to constipation: understanding the basics
Constipation is a common digestive problem. It significantly affects one’s quality of life and indicates a problem with the health of the digestive system.
Constipation is a word describing any kind of difficulties with stooling. Hard stool is one of the frequent complaints, but similarly often patients are complaining of infrequent stooling or other difficulties when trying to empty their bowels on the toilet ending up needing to spend a lot of time in the bathroom.
Stool refers to the waste matter discharged from the bowels after food has been digested. Stool forms in the large bowels or colon. Every day around 1-2 litres of bowel content arrives to the large bowel from the small intestines. In the mouth, stomach and the small intestines the food we eat gets mechanically broken down, mixed with digestive juices and chemically broken down to molecules which can pass the wall of the small intestines and enter the blood circulation to be utilised by our body. All useful elements will be absorbed and anything which cannot be digested or cannot be absorbed will pass on to the large bowel or colon. In the colon the water and salts will still be absorbed to be utilised by the body, while the shedding dead bowel cells as well as the bacteria living in the colon will add to the content made of undigestible food, eventually resulting in a neat package of waste product called stool.
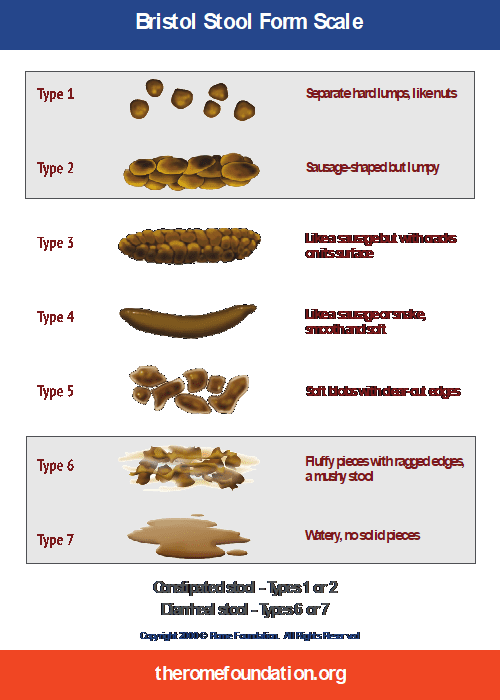
Healthy stool, as a sign of a healthy digestive system is around 150-200 grams, brown and its consistency allows it to form into a sausage shape. The Bristol stool chart describes stool consistency very well, easily understandable for patients and very informative to the doctor (see picture of Bristol stool chart). Normal stool is type 4. Type 3 and 5 are also acceptable as normal. Type 1 and 2 are abnormally hard and type 6 and 7 are abnormally loose stools.
But what causes hard stools? This problem mostly originates from dietary, lifestyle or physiological factors or the mixture of these. Insufficient fibre intake, inadequate hydration, and a lack of physical activity are the most common factors involved. These elements are crucial for maintaining the right stool consistency and ensuring smooth passage through the colon.
The inner workings: What causes hard stools?
Understanding what causes hard stool helps to address and prevent it. This condition doesn’t arise overnight but is often the result of cumulative factors related to our diet, hydration, and lifestyle choices. Let’s explore the key contributors that leads to the development of hard stools.
Dehydration
One of the most frequent causes of hard stools is dehydration, a low state of hydration of the body, caused by simply not drinking enough water! Water is a key component of the human body, making up 67% percent of it! All bodily processes happen in water. Either inside the cells, in a small pool of intracellular water. Or outside the cells in the interconnected extracellular space. Or in the blood inside the blood vessels, which is also mainly composed of water. Or inside the gut, which is actually outside place from our body’s perspective, but our digestive organs, the saliva glands, the stomach lining, the liver and the pancreas gland are pouring litres of water mixed with digestive juices into it daily to allow for digestion to happen. This pool of water in the gut allows for enough „playroom” for the food to dissolve, digestive enzymes to access it and break it down to elementary particles. Most of this water is then sucked back (reabsorbed) into the circulation along with the nutrients from our food. Ideally however some remains for the stool to be soft enough for an easy passage.
When the body is dehydrated, all these processes are underperforming.
To understand the importance of drinking sufficient amount of fluid, I always explain about daily fluid balance to my patients: In a healthy average size human body the kidneys are wishing to produce around 1500 mls of urine, to be able to put all the waste products from the blood, which are to be removed through the urine and get rid of it. With breathing and speaking we lose around 500 mls of water every day. Perspiration (sweating) accounts for some losses depending on the environment (heat, exercising, AC), which I do not even count in the equation here. And we need around 200 mls of water left for the stool. This leaves us more than 2200 mls of water to take in just to be in zero balance! If we drink less then 2200 mls our body starts sparing on the water, which we notice from the urine getting yellower or even orange colour, and the stool getting harder, climbing upwards on the Bristol stool chart.
Diet
Drinking enough is part of a healthy diet. Many patients complain of disliking water and not being able to drink litres. The good news is, that it does not need to be all water, what you drink. It can be any kind of liquid, like juices, soups, herbal teas and decaffeinated coffee, all counts fully into your water intake. Why do I write herbal tea and decaffeinated coffee? Because black tea and normal coffee are both diuretics, they make you pee more and so lose more water with the urine, sparing less for your body and bowels. So, if you do consume black tea and non-decaffeinated (i.e. normal) coffee in any forms (latte, capuccino etc also have the same amount of caffeine per serving, than espresso or americano, so it will have the same diuretic effect) then you need to drink even more liquids, to compensate for that loss. Getting back to how can we drink enough if we don’t like water: the other good news is that most fruits and vegetables have a very high water-content. If you eat a cucumber, it contains 94% water, so you think you are eating, but you are actually drinking!
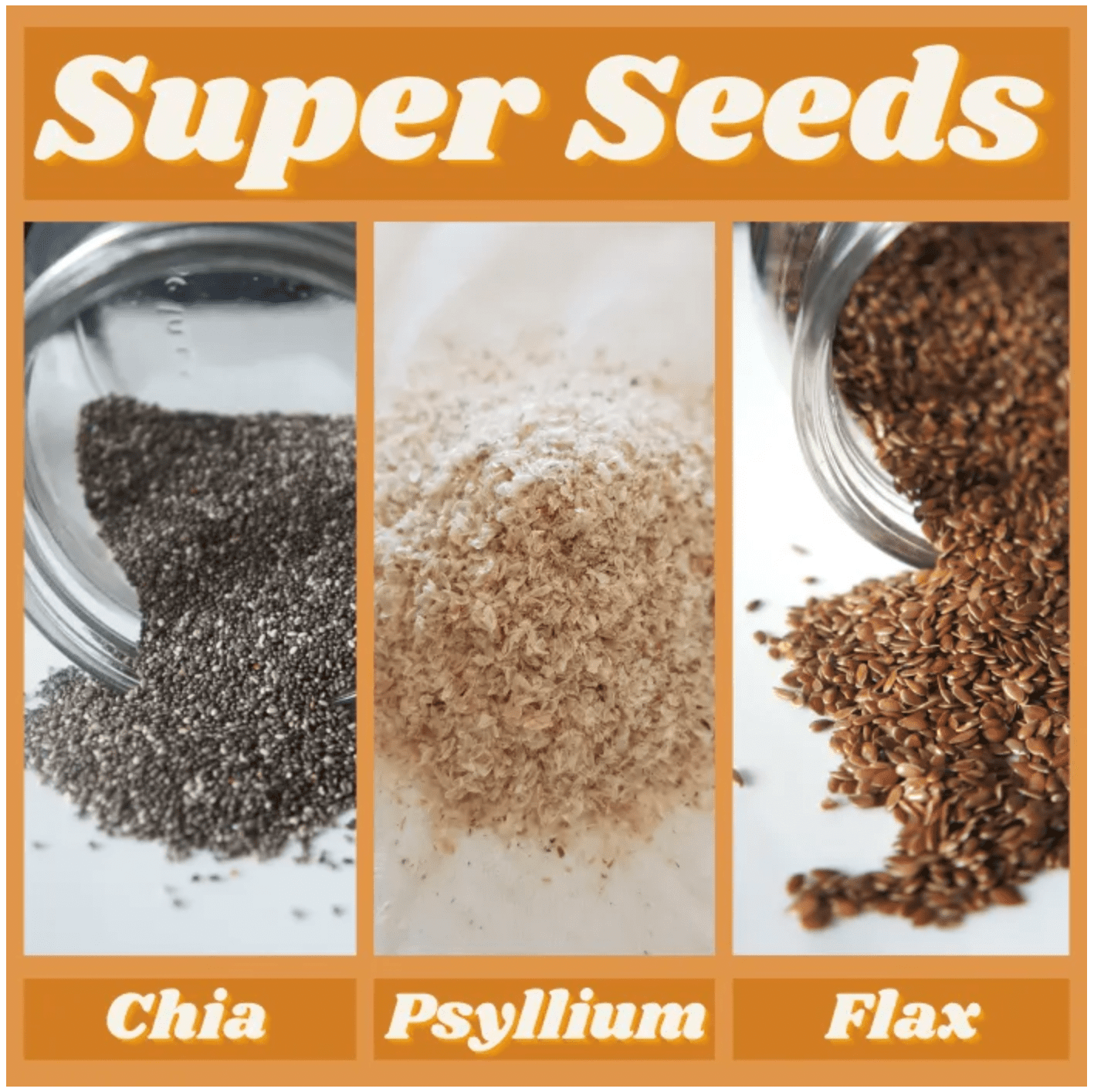
From our diet the other most important factor is fibre intake. Dietary fibres are carbohydrates, but the type of carbs, which our body cannot break down. So, fibres stay undigested in our gut. Why are they important then? They provide an amazing surface for our gut bacteria to stick to and multiply. Some of them are even feeding on it. And fibres provide a great bulk inside the colon, so the muscles of the colon wall do not need to work so hard to try and propel the stool forward. Dietary fibres are found in fruits, vegetables, whole grains, and legumes. There are amazing and even more amazing fibres in terms of achieving healthy stools. Rough fibres, like the ones in pineapples, oranges, cabbage make big bulk but less surface for the good bacteria, for some sensitive patients with irritable bowels these can cause unpleasant feeling off fullness or even crampy pain. Finer, so-called water-soluble fibres have a higher surface area, they provide more surface for food and bacteria to attach, making healthier gut flora and a more even absorption of sugars and fats. These fine fibres are found in many fruits, chia seeds, ispaghula husk etc. Fibres do not work without water however! Too much fibre with not sufficient water can even cause temporarily constipation. Properly hydrated fibres are the key to healthy diet.
Walking, exercising
Sedentary lifestyle can make the issue worse. Physical activity stimulates bowel movements by increasing blood flow and promoting contraction of the intestinal muscles. A lack of exercise can slow down the digestive process, leading to harder stools. Additionally, ignoring the urge to go to the bathroom, stress, and changes in our daily routine can negatively impact bowel movements.
In summary, what causes hard stool often boils down to a combination of dehydration, poor dietary habits, and insufficient physical activity. By understanding these key factors, patients can take proactive steps to modify their diet and lifestyle, thereby reducing the risk of hard stools and promoting a healthier digestive system.
Dietary decisions: Eating your way to softer stools
The path to alleviating hard stools often begins with what’s on your plate. Dietary choices play a pivotal role in managing and preventing this uncomfortable condition. Understanding what causes hard stool underscores the importance of dietary adjustments aimed at enhancing stool consistency and promoting regular bowel movements.
Fiber intake
A cornerstone of digestive health, fiber is essential for softening stools and facilitating their passage through the colon. Soluble fiber, found in oats, apples, and flaxseeds, absorbs water and forms a gel-like substance that softens stools. Insoluble fiber, present in whole grains, nuts, and vegetables, adds bulk and helps move food through the digestive system more quickly. Aiming for a daily intake of 25 to 30 grams of fiber from various sources can significantly improve stool consistency.
Hydration
Equally important is maintaining adequate hydration. Water works synergistically with fibre, allowing it to expand and further soften the stool. Drinking at least 8 glasses of water a day, or more if you’re active or live in a hot climate, is crucial. Incorporating hydrating foods like cucumbers, tomatoes, and watermelons into your diet can also contribute to your daily fluid intake.
Probiotics
Incorporating probiotic-rich foods like yogurt, kefir, and fermented vegetables such as Sauerkraut (sour cabbage) or kimchi can also support digestive health by enhancing gut flora. Taking probiotic supplements is another way to ensure the right balance of microbes in the gut. A balanced microbiome aids in digestion and helps prevent the formation of hard stools.
Mindful eating habits
Beyond what you eat, how you eat matters too. Eating regular, balanced meals encourages consistent bowel movements. Rushed meals or irregular eating patterns can disrupt digestive processes and contribute to hard stools. Mindful eating means eating slowly, chewing well and not allowing distraction, like TV or mobile phone to disturb the first step of the digestive process by any stress. Eating this way not only prevents hard stools but counts a lot in weight management too.
Lifestyle adjustments for better digestive health
While diet plays a crucial role in preventing hard stools, lifestyle choices are equally important in promoting a healthy digestive system. Understanding that what causes hard stool extends beyond just what we eat, incorporating certain lifestyle adjustments can significantly enhance our digestive health and mitigate issues related to hard stools.
Exercise
Regular physical activity is a key component in maintaining smooth digestive functioning. Exercise helps stimulate intestinal activity, which in turn aids in the faster movement of stools through the colon. Moderate activities, such as walking, yoga, or cycling have a profound impact on improving bowel regularity and preventing constipation.
Routine
Establishing a consistent daily routine can also play a significant role in preventing hard stools. The body thrives on regularity, and this includes the digestive system. Setting regular times for eating meals and going to the bathroom can help train your digestive system to have consistent bowel movements, reducing the likelihood of hard stools.
Stress management
Stress can have a negative impact on all aspects of health, including digestion. When we’re stressed, the body’s fight or flight response is activated, which puts digestion out of focus and lead to hard stools. Techniques such as meditation, deep breathing exercises, and mindfulness can help manage stress levels, promoting better digestive health.
Adequate sleep
Quality sleep is essential for the body’s overall health and for the digestive system to function correctly. During sleep the vegetative nerve system is mostly in parasympathetic tone, which supports digestion and restoration. Lack of sleep is a type of stress, pushing our body to the sympathetic i.e. fight or flight mode for longer hour of the day then desired. The entire digestive system is suppressed during stress, blood supply to the bowels reduces, sphincter muscles close, propulsive motion halts. Ensuring you get enough restorative sleep each night supports the body’s natural digestive processes.
Mindful bathroom habits
Listening to your body’s natural signals to use the bathroom and taking the time to do so without rushing can prevent the stool from becoming too hard. Ignoring the urge to go can cause the stool to stay in the rectum longer, leading to harder stools.
Incorporating these lifestyle changes can have a significant impact on preventing hard stools and improving digestive health overall. By focusing on regular exercise, establishing a consistent routine, managing stress, ensuring adequate sleep, and adopting healthy bathroom habits, you can support your body’s digestive system and reduce the risk of constipation.
When it is not about the hard stools – obstructed defecation type of constipation
Hard stools are difficult to pass and sometimes even unsuccessful. When the stool consistency is however not hard and stooling happens daily, but the toileting is still difficult and takes a long time, we talk about obstructed defecation type of constipation.
Patients with this problem are complaining of not being able to pass the stool, although they feel the urge, they feel the stool is there and once they do pass it, they find it to be normal or soft. Often, they can only pass part of the stool gathered in the rectal reservoir and at the end of toileting they feel stool is still there. This phenomenon we call incomplete evacuation in medical terms. Not rarely these patients have unsuccessful trials to evacuation, which means they go to toilet, because they feel the stool is there, but they do not succeed in passing any. This might happen once a month or it might happen every day.
This type of constipation cannot be fixed with improving your diet. Most of the time there is a mechanical problem behind, which needs further investigations to be revealed and physiotherapy or surgery or the combination of the two, to be solved.
When you’re stuck in the situation: “My poop is too big to come out and hurts”
Encountering a situation where it feels like “my poop is too big to come out and hurts” can be distressing and uncomfortable. If you find yourself stuck in such a predicament, knowing how to make poop come out when stuck is crucial for relief and preventing further discomfort. Here are practical tips and gentle remedies to help alleviate the blockage and encourage a smoother bowel movement.
- Drinking a glass of warm water can stimulate bowel movements. The warmth helps relax the intestines and can make it easier for the stool to pass. For added effectiveness, try adding a teaspoon of honey or lemon juice to the warm water.
- Light exercises such as walking or stretching can help get your bowels moving. Movement increases blood flow to the digestive system and can help stimulate the muscles involved in bowel movements.
- Sometimes, the position in which you sit on the toilet can impact your ability to pass stool. Using a small stool to elevate your feet and mimic a squatting position can align the rectum in a more natural angle, making it easier to pass stool.
- Deep, slow breathing, into your lower abdomen, can not only help relax the body but also relax the pelvic floor muscles, and among them the anal muscles, making it easier to pass the stool. Focus on taking deep breaths in and out to help relax your muscles.
- If natural methods are not effective, over-the-counter stool softeners or laxatives can be used as a temporary solution. It’s important to use these products as directed and not to rely on them for long-term relief.
If you frequently find yourself thinking, “how to make poop come out when stuck,” these strategies can offer relief. However, it’s important to address the underlying causes of hard stools to prevent reoccurrence. Should the problem persist, or if you experience significant pain, bleeding, or other concerning symptoms, consulting your doctor is recommended.
Medical treatment – over-the-counter medications and when to use them
When dietary and lifestyle changes are not enough to alleviate hard stools or when you’re in a situation mentioned above, where you think “how to make poop come out when stuck,” over the counter laxative supplements/medications can provide relief. It is important to understand the different types of laxatives available to choose the right one for the right problem.
Stool softeners
Stool softeners, such as docusate sodium, work by reducing surface tension (detergent) hence increasing the amount of water the stool absorbs inside the gut, making it softer and easier to pass. Stool softeners are gentle and suitable for short-term use. They do sound innocent, but long term and excessive use can lead to electrolyte imbalances and dependence!
Bulk-forming laxatives
Bulk-forming laxatives, like psyllium, methylcellulose, and polycarbophil, work by absorbing water in the intestine to form a soft, bulky stool that’s easier to pass. They come closest to a healthy dietary change to fix constipation. They are safe to take even for long-term. However, they require adequate hydration to be effective.
Osmotic laxatives
Osmotic laxatives, including polyethylene glycol and lactulose, draw water into the bowel to soften the stool and stimulate bowel movement. They are also safe and effective, and they would even work if water intake were not sufficient, kind of forcefully hydrating the stool on the expense of the body. This explain why they should not be used long term unless adequate hydration is ensured.
Stimulant laxatives
Stimulant laxatives, such as senna and bisacodyl, act on the mucosal lining of the colon and its nerve plexus by stimulating secretion of higher volume of mucus, water and electrolytes as well as increasing intestinal motility resulting in a faster passage of stool along the gut. They are effective for immediate relief but should be used sparingly, as frequent use leads to dependency and decrease bowel function over time.
Laxative medications are effective for relieving hard stools and constipation, but they should be used responsibly. Always consider them as a temporary solution while working on underlying dietary and lifestyle changes for long-term digestive health.
Disease which originates from constipation
Constipation being a health problem by itself, can also lead to further problems and diseases if not sorted out in time.
Hard stools can break up the anal lining, causing acute anal fissures, if circumstances align extra stress and/or a sensitive, thin and dry skin chronic anal fissure can develop, which sometimes can only be sorted with surgery.
Chronic straining at stools can lead to prolapsing hemorrhoids in a few years, rectal lining prolapse and even prolapse of the rectum itself if goes on for many years and is coupled with loose connective tissue and/or sudden weight loss.
All these diseases can be prevented with a healthy diet rich in fibers and water, regular low impact exercise and a mindful toileting habit.
Long-term strategies for preventing constipation
Preventing constipation requires a comprehensive understanding of its causes and a commitment to adopting healthier dietary and lifestyle habits.
A diet incorporating a variety of fruits, vegetables, whole grains, and legumes can significantly improve stool consistency. Fibre works by absorbing water, which softens the stool and makes it easier to pass. Equally important is staying well hydrated. Water is essential for fibre to function effectively and for keeping the digestive system running smoothly.
Regular physical activity stimulates the digestive system and enhances bowel movements, preventing constipation and hard stools. Establishing a routine, including fixed times for eating and using the bathroom, can also help regulate bowel movements.
Managing stress through mindfulness, exercise, or hobbies can positively affect digestive health. Stress can disrupt digestive processes, leading to hard stools, so finding effective ways to relax and decompress is crucial.
Regular consultations with healthcare professionals can help catch and address any underlying issues that may contribute to hard stools. Early intervention can prevent complications and guide you toward the best preventative measures tailored to your health profile.
In summary, constipation is more frequently a „bad habit” then a disease or a way one is made up. With healthy lifestyle, mindful eating habits and an attention to our body it can be treated or prevented. Living with constipation is a daily struggle significantly reducing life quality. In the long term it leads to health consequences, diseases and even surgeries. Incorporating the above simple strategies to our everyday life can be a game changer, resulting in a healthier, happier life.