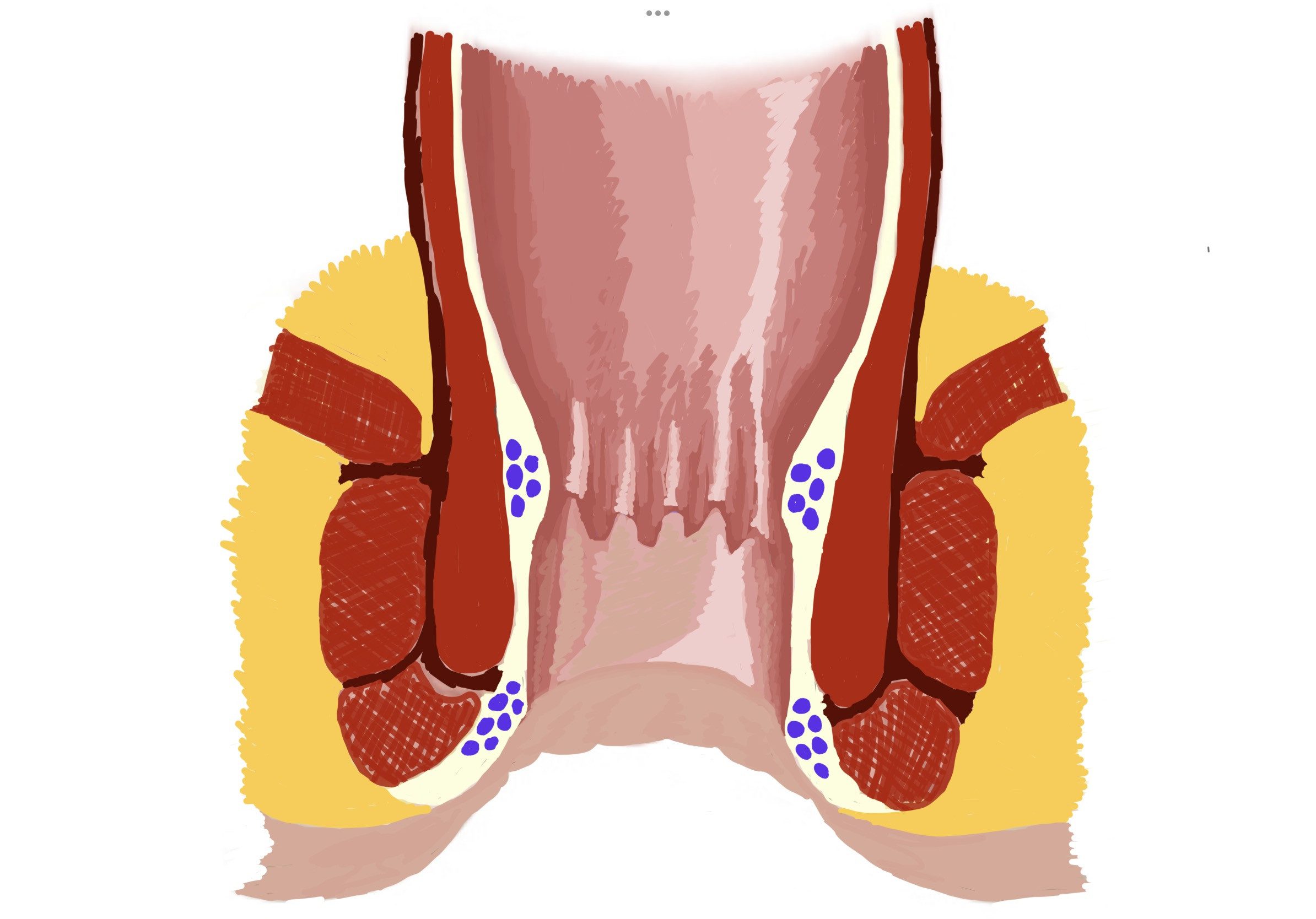
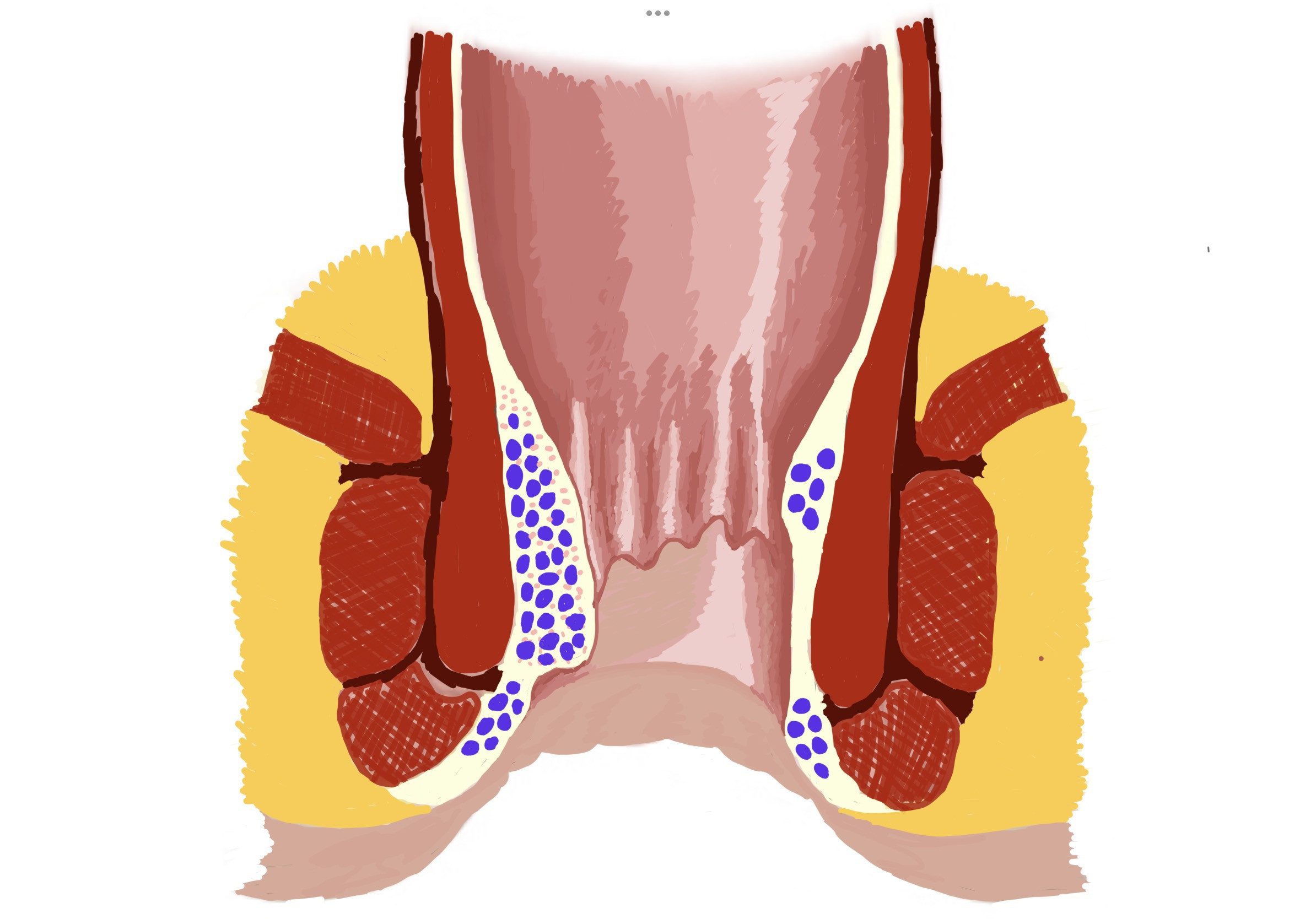
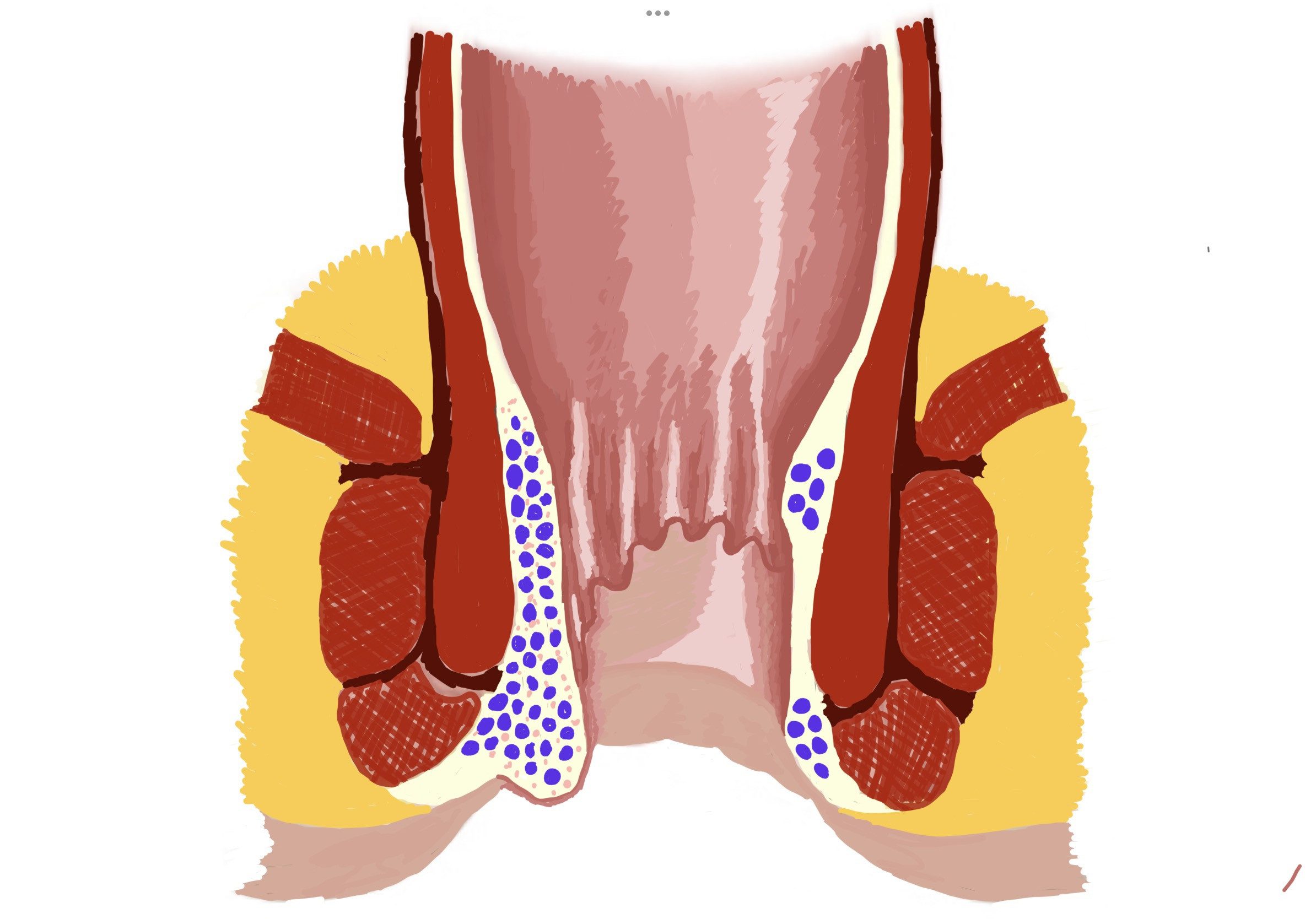
Hemorrhoidal cushions are part of normal anatomy. They are responsible for the fine tuning of the closure of the anal opening. We have internal and external hemorrhoidal cushions, at the top of the anal canal covered with mucus membrane and at the entrance of the anal canal covered by anal skin.
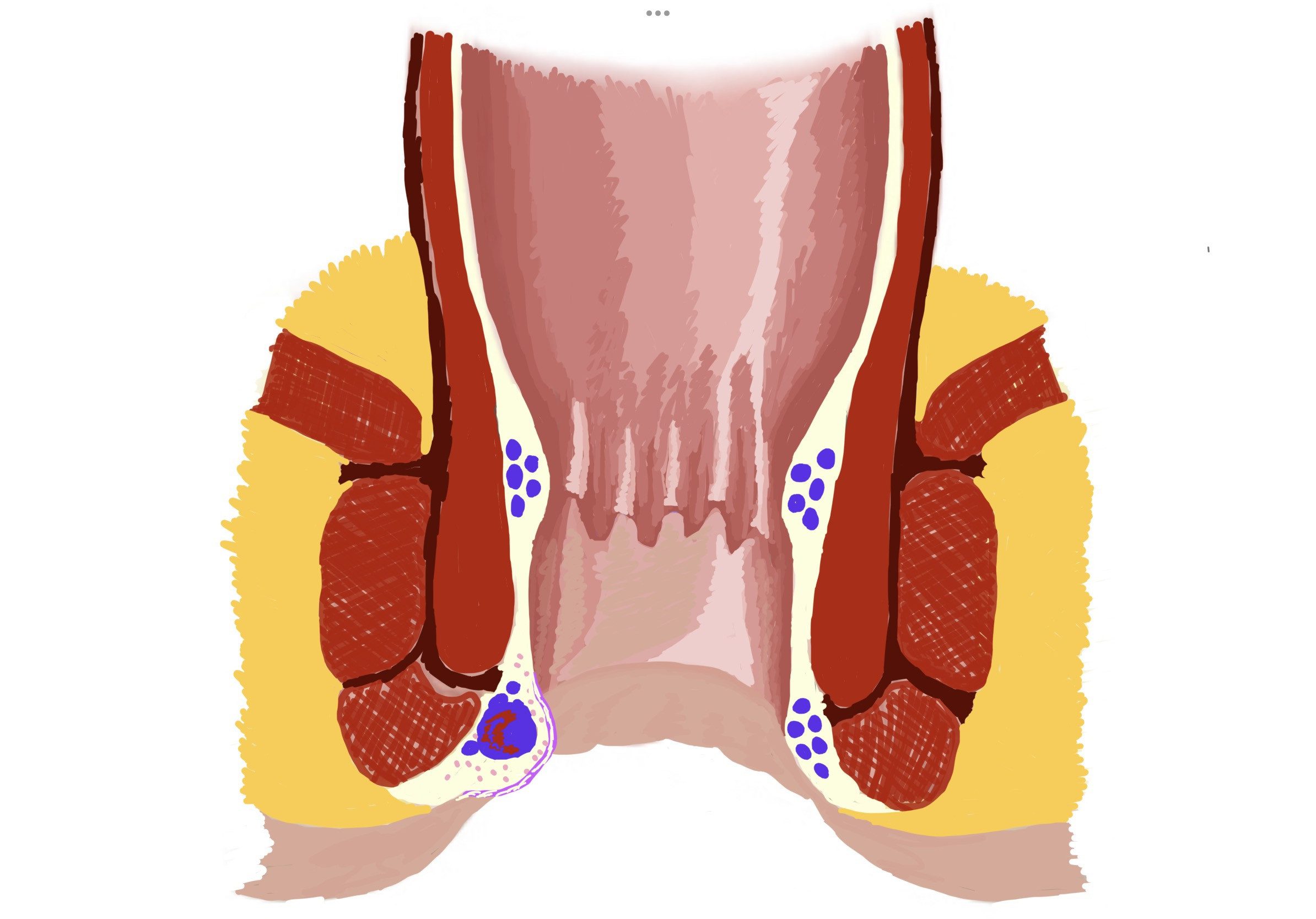
We only call them Hemorrhoids as a disease, when they become enlarged, prolapsing or some complication, like bleeding or thrombosis, happens to them. These complications, called hemorrhoidal flare-ups cause pain and swelling and normally settle in a few days or weeks on conservative treatment with suppositories or ointments.
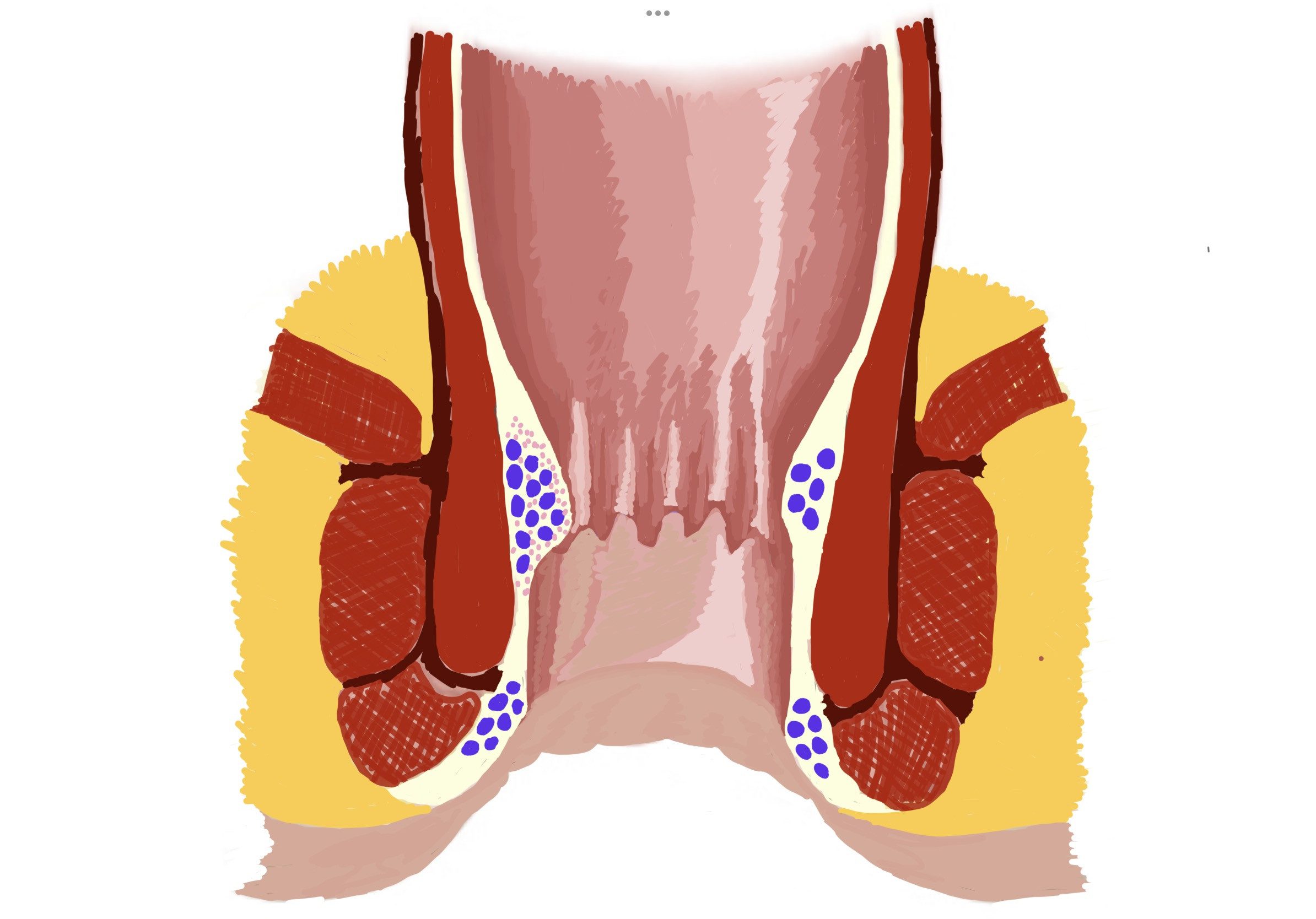
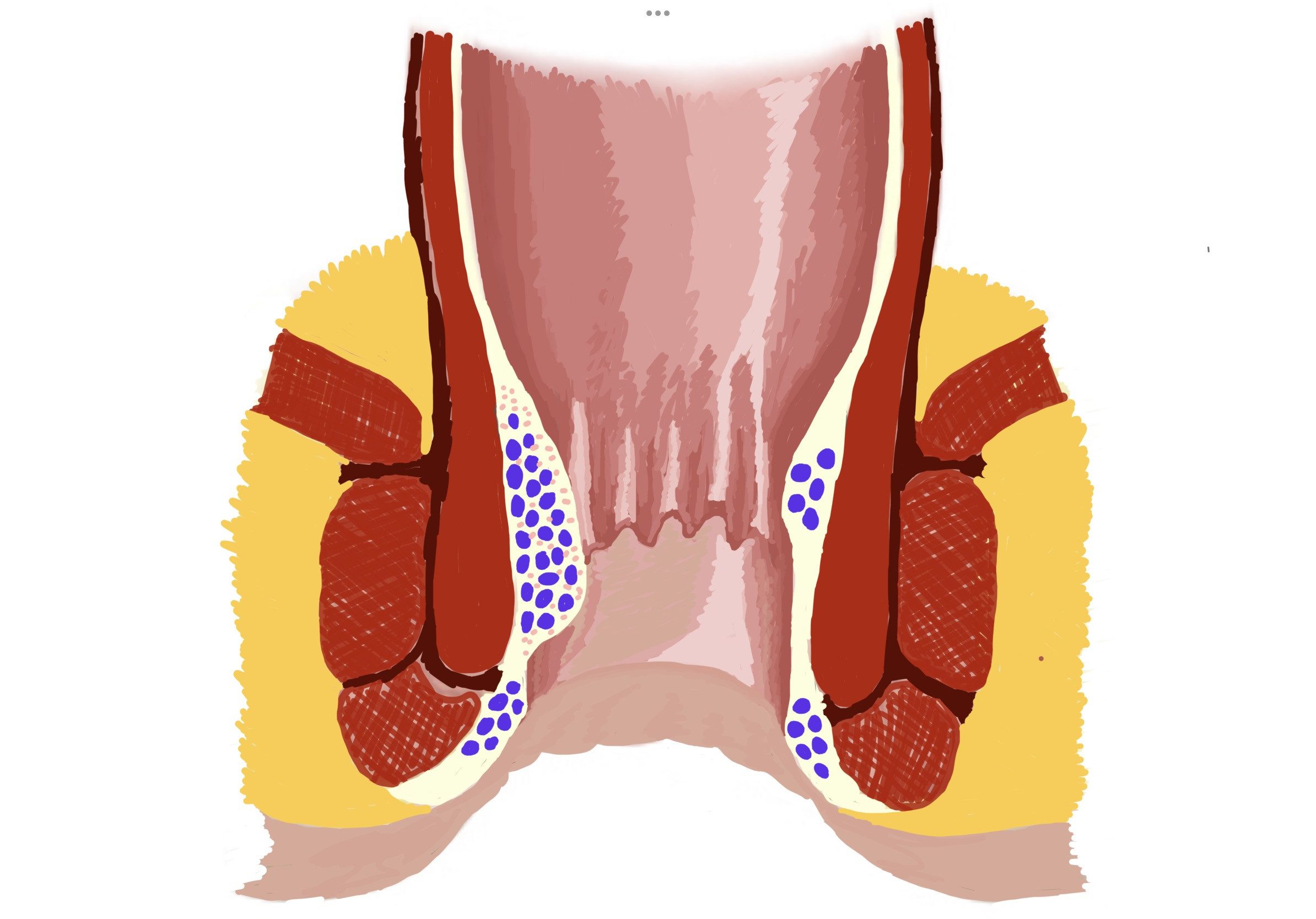
Ongoing straining at the toilet, long hours of sitting, constipation, pregnancies etc. can contribute to enlargement and gradual prolapse of the internal hemorrhoidal cushions (graded from 1 to 4). This progressing hemorrhoidal prolapse process takes several years and might be not painful at all. More often symptom free periods alternate with hemorrhoidal flare ups. The flare ups start from a bad diet causing constipation or diarrhea or from unusual physical exertion. They settle by themselves or on conservative anti-hemorrhoidal treatment, which means the inflammation goes down, the pain subsides, bleeding stops, but the underlying prolapse will not reverse.
Since the resulting advanced hemorrhoidal disease cannot be reversed with conservative treatment, in advanced, grade 3, grade 4 cases hemorrhoid surgery is suggested. Grade 2 hemorrhoids might also need surgery, if they bleed too much or flare up so frequently that it significantly interferes with every day quality of life.
What signs and symptoms one has with this problem?
Hemorrhoids typically cause anal dyscomfort, internal hemorrhoids might bleed, external hemorrhoids present as a constant lump, prolapsing hemorrhoids come out with defecation and depending on the grade they return back to the anal canal after toilet. Strong pain is not typical of hemorrhoids unless they are thrombosed.