- Home
- /
- Hemorrhoid and Anal Fissure...
LPH (Laser Hemorrhoid Procedure)
LPH or Laser Hemorrhoid Procedure is the least painful surgical method to treat hemorrhoids. It comes with so much less pain then traditional hemorrhoid surgeries, that it does not need general anesthesia, but can be performed with deep sedation and local anesthesia only and with fast recovery.
During the procedure a laser probe is introduced through pinpoint incisions just outside the anal opening and navigated under the external and internal hemorrhoid cushions, laser energy is applied to coagulate the hemorrhoid vessels and attach the prolapsing cushions back to the muscle wall of the anal canal. This method is much less painful than any other method of hemorrhoid surgery. Laser creates a light, controlled burning of the hemorrhoidal vessels. After the surgery there comes a short inflammatory phase, which can be uncomfortable for 3-5 days, then a longer, 6-8 weeks regenerative phase comes, which however is going on in the background while the patient can return back to her/his normal life. This tissue regeneration restores normal size of hemorrhoidal cushions. For the procedure the patient spends only 4-6 hours at the daycare center. The downtime is 3-5 days depending on patients pain tolerance and how advanced the hemorrhoids are.
Advantages: least painful, fastest recovery
Limitations: by itself only handles grade 2, early grade 3 hemorrhoids
Hemorrhoidopexy
Hemorrhoidopexy means suturing/fixing up the falling (prolapsing) hemorrhoids and shrinking their blood supply. Since normal size hemorrhoidal cushions are part of normal anatomy, this surgery restores normal anatomy instead of cutting away or destroying the hemorrhoid cushions.
Hemorrhoidopexy is much less painful than hemorrhoidectomy.
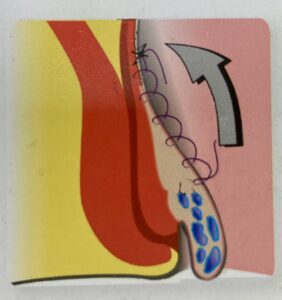
There are two main ways of doing it: suturing with surgical threads or stapling with a surgical circular stapler. The suturing method’s medical name is transanal hemorrhoidal dearterialization and rectal mucopexy. It involves individually finding and suturing the supplying artery to the three primary and three secondary hemorrhoidal cushions then suturing up the hanging mucus membrane again in 6 positions.
The stapling machine method is called stapled hemorrhoidopexy and it involves stapling up the hanging mucus membrane along with the hanging hemorrhoid cushions in a circumferential fashion and with the same staple line disconnecting their blood supply.
If external components (outside tags) do not reduce properly by the pulling-in forces of the hemorrhoidopexy, they either remain there or need to be cut traditionally.
Hemorrhoidectomy
Hemorrhoidectomy is the old fashioned and well-established way of operating hemorrhoids: cutting them away.
It can be performed by scalpel, electrocautery, ultrasonic cutting device etc. Either way it results in wounds – normally three – running up the whole length of the anal canal. The wounds can be left open (Milligan-Morgan Hemorrhoidectomy) to avoid complications of the inevitable infection from stool bacteria, or they can be closed with sutures (Park’s or Ferguson Hemorrhoidectomy) with the intention of faster healing.
Traditional hemorrhoidectomy is still considered the gold standard surgical treatment of hemorrhoids by most medical universities. This surgery is however the infamous surgery, which is responsible for the bad reputation of hemorrhoid procedures. It is very painful indeed. Patients often describe the experience of going to the toilet after this surgery as passing knives.
Nowadays we try to avoid traditional hemorrhoidectomy, but in case of large and fixed external components, at least part of it still needs to be performed.
Combined Hemorrhoid Procedures
We have six hemorrhoid cushions, three primary ones at 3, 7 and 11 o’clock and three secondary ones in between. It is very unlikely that they are all affected the same way by the disease called hemorrhoids (hemorrhoidal engorgement, hemorrhoidal bleeding, hemorrhoidal thrombosis, hemorrhoidal prolapse). Grade 2 and early grade 3 hemorrhoids can be fully treated with laser, grade 3-4 hemorrhoids need the prolapse to be undone by pulling up with hemorrhoidopexy procedures, while fixed prolapses which would not move back on pulling as well as solely external components (outside piles) needs cutting.
Therefore in reality many hemorrhoid surgeries are the combination of the above methods to achieve the best result with the least pain for the patient’s best outcome.

Fissurectomy
Fissurectomy is the name for the surgeries we make for anal fissures, if they failed to heal on conservative treatment. Nowadays we avoid cutting out the fissure, because its base is made of muscle, so the “ectomy” in the name, referring to cutting, is outdated. Instead of cutting we rather focus on relaxing the anal sphincter muscle, mostly by Botox injection. If any cutting is involved, it is limited to the skin tag.
In case this kind of “conservative operation” is not sufficient to heal a fissure, and the patient’s internal anal sphincter is long and robust, rarely, sphincterotomy is done, which is relaxing the lower part of the internal anal sphincter by a cut. This is permanent, unlike the Botox injection, so we try to avoid it.