Introduction to Anal Abscess
Anal abscess is an acute (suddenly occurring), painful anal condition that may affect anyone regardless of age, gender, social status or whereabouts in the world. Abscess – anywhere in the body, not only in relation to the anus – means the formation of a tissue pocket filled with pus. Pus formation is the response of our immune system to bacterial invasion to the otherwise normally sterile tissues of the body. Anal abscess is a very painful and potentially dangerous disease. Having an idea of the nature, causes, and treatment of anal abscess is important for anyone suffering from it to understand why cooperation with the treatment is vital. This article will go over what an anal abscess is, its causes, symptoms, and treatment. By the conclusion, you will have an understanding of this ailment and how to effectively get it treated.
Understanding the Anatomy: What is an Anal Abscess?
The human anatomy around the rectum and anus is rather complex and can be broken down to the outside world, gut lumen and inner world. The outside world is getting in touch with our body through the skin, which covers our buttocks and creeps in the anal canal as high as 2-2.5 cms up until the middle of the anal canal. The skin has its own bacterial flora, mostly streptococcus and staphylococcus bacteria living there, and it has thousands of tiny glands as well as hair follicles. Hair follicles are spread out and are plenty on the skin of the buttocks, but they do not exist on the specialised skin of the lower anal canal and immediate perianal area just outside the anal hole. This special skin is called anoderm. It is thinner than the normal skin and very sensitive. The gut lumen is immunologically also outside, however we do not see it, it is our “folded-in outside” world, where the digestive process takes place. Its lower part, the rectum and anus are covered with mucous membrane with plenty of glands, and mostly coliform bacteria (Escherichia coli) are living there. The mucous membrane descends from the rectum down to the upper anal canal and meets with the anodermal skin halfway in the anal canal at a wavy line called the dentate line.
The true inner world is what is between the skin and the mucous membrane and here it consists mostly of the anal sphincter muscles, pelvic floor muscles, rectal wall bowel muscles and connective tissue separating these. The true inner world is sterile and is guarded by immune cells, the soldiers of the immune system. There are a few (around 8-12) large, mucus producing glands in the middle of the anal canal, at the dentate line, where the anodermal skin and the mucous membrane of the rectum and upper anal canal meet. Their job is to lubricate the lower anal canal for the stool to slide out easily.
Most of the anal abscesses develop from these glands, when they get clogged and their content cannot empty and gets infected by local bacteria. Some anal abscesses develop from fissures and ulcers of the anal canal and rectum if these wounds are getting too deep, crossing the barrier to the inner world and allowing the local bacteria to invade the inner tissues. The immune system reacts to these infections and tries its best to localise the bacteria to one spot by creating, oedema, swelling in the vicinity, flushing the area with blood to drive immune cells there, building a fibrin wall around the invasion and kamikaze-killing the bacteria (Did you know that pus is mostly made up of immune cells killing bacteria and dying themselves in the process). This inflammatory process in response to bacterial invasion increases the pressure in the tissue and allows the pocket of pus to slowly migrate closer to the surface and eventually burst out through the skin. This is a very important immunological process, which saved the life of our ancestors many times during the past hundreds of thousands of years. Abscess formation and its emptying effectively saves us from sepsis (bacteria invading the blood and threatening the whole body). This process is easy if the bacterial invasion and the abscess develops on a relatively simple area of the body. For example a thorn scratches the skin of the arm or leg a little too deep resulting in a skin abscess. An abscess however originating from the middle of the anal canal is developing in an area with a rather complex. In this delicate area spontaneous or surgically guided resolution of an abscess can result in more or less troublesome consequences.
Gaining a little insight into the anatomy of the perianal area helps understanding the complexity of this disease and its treatment.
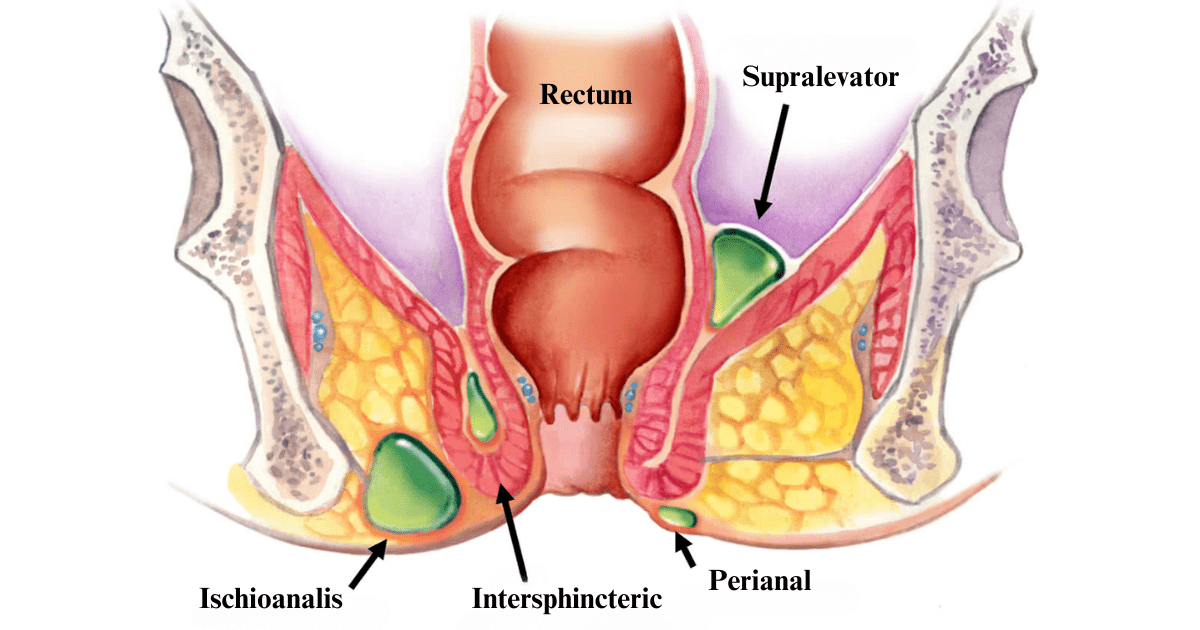
Different Anal Abscesses Based on Location
Abscesses around the anus and rectum can be perirectal or perianal. Perirectal (supralevator) abscesses are rare and are related to serious disease processes, like abdomino-pelvic infections, severe Crohn’s disease, malignancies, fistulating rare infections, complications of radiotherapy.
Perianal abscesses are much more frequent, they are limited to the vicinity of anal canal and are always situated below (rarely below plus directly above) the levator ani muscle (muscle sheet of the pelvic floor). They are further divided into groups depending on their location compared to the anal sphincter muscles (namely the external anal sphincter muscle and the internal anal sphincter muscle). This grouping is important for its therapeutic consequences. Superficial subcutaneous anal abscesses are directly under the anodermal skin, normally very close to the anal opening. They are very obvious and easy to drain. Intersphincteric abscesses are between the internal anal sphincter and external anal sphincter. Since this location is very tight and hidden, they are very painful and difficult to diagnose, unless the doctor suspects this problem. Ischiorectal (correctly ischioanal) abscesses are beyond the external anal sphincter muscle ring, in the fatty tissue around the anal canal. There is a larger soft space for them to grow there, so they can grow bigger and relatively deep before the pain takes the patient to visit the doctor.
Common Symptoms of Anal Abscesses
Pain is the leading symptom of an anal abscess, however pain here can signify many other things, like anal fissure, thrombosed hemorrhoid or anal spasm from psychological distress. Lump or swelling felt around the anus is the second most important sign, which again has a long list of differential diagnoses. However a round painful lump with redness of the overlying skin would be more specific to an anal abscess.
The intensity of pain caused by an anal abscess can range from moderate to severe, throbbing pain. It might intensify during bowel movements or when sitting. Additionally, the affected area may be tender to touch and display signs of redness and swelling. Fever and chills can accompany these local symptoms, if the abscess is large and deep.
If the abscess persists long enough without the patient seeking treatment, it might burst by itself, causing a purulent (pus containing), rather bad smelling discharge. Once the abscess empties, the pain reduces considerably.
It is important to go to the doctor early, if you suspect you have an anal abscess, because potentially dangerous spreading infection can develop. Patients are at risk of dangerous infection if their immune system is compromised or in case the causing bacteria harbours some special enzymes to break down immune barriers.
Causes of Anal Abscess
One of the primary causes of anal abscesses is the infection of the above mentioned anal glands, opening in the middle of the anal canal. These glands produce mucus. The mucus passes through a narrow tube (duct) to empty inside the anal canal. In case this tube gets blocked, bacteria can accumulate, resulting in an infection and eventually an abscess.
Deep anal fissures can also be the cause for bacteria finding their way to deeper tissues. Abscesses from anal fissure form in the midline of the body, in the front or the back of the anal opening, close to the surface and they form the superficial type of abscesses.
Perirectal (supralevator) abscesses form from more serious pathologies, like deep ulcers or fistulas os Crohn’s disease, infective complications of diverticulosis, ulcers from radiation proctitis. Rarely they can form from upward spreading anal abscesses.
Trauma or injury to the anal area, including surgical procedures, can also pave the way for bacteria to enter the tissues, leading to an abscess.
Individuals with a compromised immune system, such as those with diabetes or HIV, are at a higher risk or developing abscesses.
Although not a true perianal abscess – skin abscesses of the surrounding area, i.e. the skin of the buttocks, can sometimes be mistaken as anal abscesses and pose an important group of differential diagnoses. Skin abscesses can develop on any part of the body from infection of one of the millions of skin glands we have. Better known as pimples, skin abscesses sometimes can grow larger and can look like an anal abscess. The main difference is the causing bacteria: skin abscesses are caused by the normal flora of the skin, namely Streptococcus and Staphylococcus bacteria, while anal abscesses normally contain stool bacteria (mostly Escherichia coli). Treatment of skin abscesses is simpler and there is no risk of formation of anal fistula after they have emptied spontaneously or got drained surgically.

Diagnosing Anal Abscesses: What to Expect
When suspecting an anal abscess, it’s essential to seek medical advice promptly. Early diagnosis can pave the way for effective treatment and prevent complications. It is also very important to visit the correct speciality with this problem: you are best off to visit a Proctologist. If you see a Gastroenterologist or a Family Medicine Doctor, they should also point you in the right direction. In many places there are no Proctology specialists available and you will find that proctological problems like anal abscesses are treated by General Surgeons just as well.
Here’s what to expect at your visit:
- Medical History: The doctor will ask questions about your symptoms, their onset, and any potential risk factors. This includes previous medical conditions, surgeries, or injuries to the anal region.
- Physical Examination: The primary method for diagnosing an anal abscess is through a physical examination. A healthcare professional will inspect the anal area for signs of swelling, redness, and tenderness. They may also palpate (feel) the area to determine the depth and extent of the abscess.
- Imaging Tests: For deeper abscesses, like a ischioanal/ishiorectal or supralevator perirectal abscesses, imaging tests are absolutely necessary. For the more superficial anal abscesses it is also very helpful to have an imaging test, however not always necessary. Anal Canal MRI (magnetic resonance imaging) or Endo-Anal Ultrasound Scan are the two modalities, which gives precise enough visualisation of the abscess’s location, size and relation to the anal and pelvic floor muscles.
- Laboratory Tests: If the abscess is large and there is general unwellness, fever and other symptoms affecting the whole body, blood tests are taken to check for the inflammatory markers. This determines how serious, how acute the problem is, helps to see how much your whole body might be involved in the inflammatory response or your immune system managed to localise the infection. In some cases, a sample of the pus might be taken for microbiological testing. This can help identify the specific bacteria causing the infection, guiding the treatment process.
While the idea of a medical examination in such a sensitive area might be daunting, your doctor will make sure to handle the situation with maximum gentleness and discretion to ensure your well-being and guide you towards the best possible outcome.
Treatments: Surgical and Non-Surgical Options
Once diagnosed with an anal abscess, your doctor will explain to you the available treatment options. The approach to treatment largely depends on the size, location, and severity of the abscess.
- Surgical Drainage: “Ibi pus ubi evacua” says the Latin teaching which still applies in most of the cases. It means, where there is pus, it needs to be drained. If the abscess did not burst by itself, surgical drainage is a must. The procedure involves making a small incision to drain the pus from the abscess. To avoid pain it is done under general anaesthesia or sometimes local anaesthesia depending on the size and depth of the abscess and on the patient’s preference. Surgical drainage empties the collection of pus and cleans the cavity to allow it to shrink over time. It relieves the pain very effectively. No closure of the drainage wound should be done at this point, otherwise the abscess comes straight back. The infected tissues have to settle, which takes a few days and comes with a bit of discharge, needing you to apply some dressing or pad, which your doctor will explain to you. You also need to attend for follow up(s) to ensure the cavity is closing from the depth and not from the surface. If the skin closes first, infected deeper tissue can remain behind and the abscess recurs.
- Antibiotics: Antibiotics are almost always prescribed to protect your body from spreading infection, however, antibiotics without drainage of the pus collection is not sufficient to achieve cure in the vast majority of cases. There are some very rare situations when a small abscess is at such a tricky place, that drainage would have high chances of complication, your doctor might decide to weigh the risks and benefits and give it a try to heal you with antibiotics only. This however is very rare and needs a close follow-up to change the plan of treatment in time, if necessary.
- Follow-up Care: After surgical drainage regular check-ups are essential to ensure the abscess is healing correctly, to prevent recurrence. At this stage your doctor will have a chat with you about anal fistulas. True anal abscesses have a high chance of “healing into an anal fistula”, no matter what. Regular follow-up and wound care ensures the abscess to heal up in a straightforward way, however if its connection to the lumen of the anal canal through the remnants of the infected anal gland persists, unfortunately it will end up as an anal fistula even with the best possible care. It takes a few weeks to a few months to find out if an anal abscess was a one off happening and the patient can forget about it as a “bad memory” or it comes back as an anal fistula or recurring anal abscess in which case anal fistula surgery will be needed.
In conclusion, anal abscess is a proctological urgency, which almost always needs surgery. If you believe you are showing the signs of an anal abscess do not delay seeking medical treatment. The best specialist you can go to for your treatment is a proctologist, who is well trained to treat you as gently as possible, and to explain to you the disease process, your treatment options and the expected outcome.
 Recovery and Aftercare Post-Treatment
Recovery and Aftercare Post-Treatment
The period following the treatment of an anal abscess is crucial. Proper aftercare can ensure a swift recovery and minimise the chances of complications or recurrence.
Wound Care:
If you’ve undergone surgical drainage, it’s essential to keep the area clean and dry. Regularly changing dressings, as instructed by your healthcare provider, will prevent further infections and aid in healing.
Sitz Baths:
Hot/warm sitz bath is NOT advised in case of inflammatory and infective processes. It would increase swelling and potentially make you suffer more. Luke-warm (body temperature) sitz bath with Epsom salt has many advocates. Indeed the bath salt can help pull down the oedematous swelling accompanying the abscess. In some inflammations applying ice pack can help with the pain, however cold can increase the muscle tone which is again not the best idea if the abscess is close to the anal opening.
Medication:
Your doctor will prescribe painkillers until you wait for your procedure and to manage discomfort post-treatment. If antibiotics are prescribed, ensure you complete the entire course, even if you feel better.
Dietary Considerations:
A high-fiber diet can help in preventing constipation, which is essential as straining during bowel movements can be painful and hinder the healing process.
Regular Check-ups:
Post-treatment, routine visits to your healthcare professional are vital. They will monitor the healing process, ensuring there’s no recurrence of the abscess.
Recovering from an anal abscess requires patience and compliance. By following your doctor’s instructions and maintaining open communication with your healthcare provider, you can ensure a smooth recovery and return to your daily routine with confidence.

Complications and Risks
Anal abscess, if remains untreated might burst by itself, and if it was small and superficial might as well heal. Very few anal abscesses however are so lucky to fall in this category.
Larger and more deeper abscesses without treatment can spread around the anus in a horse-shoe shape fashion, causing complicated disease which is more difficult to handle at a later stage.
Other than spreading vertically, they can also spread upwards towards the deeper tissue especially if patients are continuing sitting while taking painkillers to put up with the pain. This type of delay can result in high and complex abscesses which eventually open at more than one hole to the outside world resulting in multiple fistulas.
If the immune response is compromised, or the bacteria involved in the abscess formation are particularly aggressive, dangerous spreading infection can develop with very severe, life threatening complications. This is a rare scenario, however it does occur.
Abscesses in the buttocks, if left untreated, can grow in size and cause increased discomfort and pain. Most abscesses would eventually rupture spontaneously, but if they are large and deep, they will not empty completely, causing recurrences of abscesses or chronic discharge at the site of the rupture, which is called a fistula.
Unfortunately even with the best possible care fistula formation is a frequent complication! This is very important to know. The reason for this, is that the abscess is originating from an infected gland connected to the anal canal. Once the whole infection inflammation settles, the gland’s duct might reopen and allow anal content to enter to the site of the abscess and leave at the site of the drainage. You can read more on anal fistula formation, its causes and its treatment at the Anal fistula chapter and Anal fistula treatment chapter.
In conclusion, while the prospect of treating an anal abscess might be daunting, the potential complications of leaving it untreated are far more severe. Seeking timely medical intervention and following recommended treatments can prevent these risks and ensure the best outcome.
Conclusion and Recommendations
The journey of understanding and addressing any type of anal pain, potentially an anal abscess, is undoubtedly challenging, given the sensitivity and discomfort of the condition. However, armed with the right information and a proactive approach to treatment, individuals can navigate this health concern effectively and regain their well-being.
An anal abscess requires prompt attention. Delaying treatment or ignoring symptoms can lead to more severe complications, making recovery longer and more complex. It’s essential to prioritise one’s health and seek medical guidance at the early signs of an abscess.